Glaucoma
Preserve your vision with early detection & treatment
Have Any Query?
Enter Your Mobile Number For Call back
What is Glaucoma?
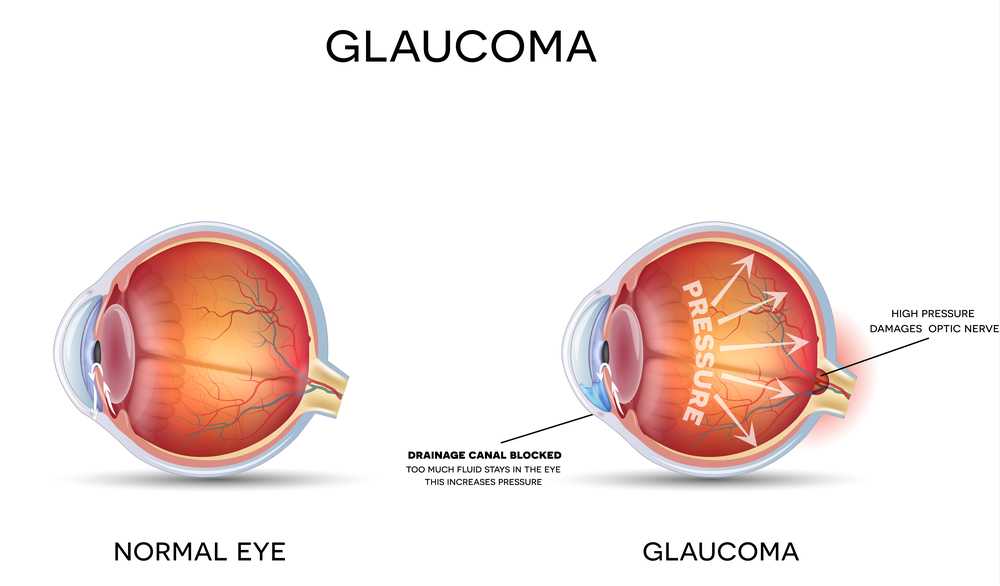
Glaucoma or Kala motia is a sight threatening group of diseases in which there is damage to the optic nerve caused by increased pressure within the eye. It is known as the ‘Sneak Thief of Sight’ since you could lose vision without knowing until it is too late. It is a serious condition that must not be ignored, early diagnosis and regular treatment is the key to saving your sight.
Are you at risk for Glaucoma?
Age> 45 years
Family history of Glaucoma
Diabetes
Hypertension
Myopia (Nearsightedness)
Hypermetropia (Farsightedness)
Prolonged Steroid use
Blunt injury to the eye

Symptoms of Glaucoma
In the early stages there are no obvious symptoms. By the time the patient becomes aware of decreased sight, the damage is already quite advanced. Hence, it is important to have regular eye check ups especially over the age of 40 years. Depending on the type of Glaucoma ( Open or Closed angle) following symptoms may occur
- Gradual, painless loss of vision
- Halos around lights
- Headache or browache
- Nausea with severe eye pain
- Blurred vision at night
- Loss of side/ peripheral vision
How is Glaucoma diagnosed ?
The best way to detect early Glaucoma is by a complete eye check up by your Eye specialist. This includes checking your vision, your intraocular pressure (IOP), evaluating the drainage angle of the eyes and examining your Optic nerve. If you have a risk factor for glaucoma, raised eye pressure,narrow angles or abnormal appearance of the Optic Disc,you will be advised to take certain special tests.

Glaucoma Investigations - Basic Test
Measurement of the eye or Intraocular pressure (IOP) is essential and needs to be monitored regularly. Like Blood pressure, eye pressure can vary at different times of the day. Normal IOP is < 21mm Hg. It can be measured by Contact or Noncontact methods. The most accurate technique is by Goldmann Applanation Tonometry.
Examination of the drainage angle of the eye by a special contact lens, the 2 or 4 mirror Gonioscope. By this one can know the type of Glaucoma -Open Angle or Closed Angle, Angle recession due to injury or Neovascular (formation of new blood vessels in the angle) etc. After anaesthetising the eye, the contact lens is held in place over the eyeball and the angle is then viewed under high magnification.
Evaluation of the Optic Nerve and Retinal nerve fibre layer is done by using 90D biomicroscopy or Indirect Ophthalmoscopy. Eye is usually dilated for a better view.Red free filter is used for further refinement.
Measurement of the corneal thickness as it affects the accuracy of IOP readings. Thicker corneas estimate higher IOP, while thinner corneas underestimate IOP. Hence a correction has to be factored in depending on the Pachymetry. Average pachymetry is 520-540 microns. It is a quick,simple, painless test.
Measurement of the eye or Intraocular pressure (IOP) is essential and needs to be monitored regularly. Like Blood pressure, eye pressure can vary at different times of the day. Normal IOP is < 21mm Hg. It can be measured by Contact or Noncontact methods. The most accurate technique is by Goldmann Applanation Tonometry.
Examination of the drainage angle of the eye by a special contact lens, the 2 or 4 mirror Gonioscope. By this one can know the type of Glaucoma -Open Angle or Closed Angle, Angle recession due to injury or Neovascular (formation of new blood vessels in the angle) etc. After anaesthetising the eye, the contact lens is held in place over the eyeball and the angle is then viewed under high magnification.
Evaluation of the Optic Nerve and Retinal nerve fibre layer is done by using 90D biomicroscopy or Indirect Ophthalmoscopy. Eye is usually dilated for a better view.Red free filter is used for further refinement.
Measurement of the corneal thickness as it affects the accuracy of IOP readings. Thicker corneas estimate higher IOP, while thinner corneas underestimate IOP. Hence a correction has to be factored in depending on the Pachymetry. Average pachymetry is 520-540 microns. It is a quick,simple, painless test.
Advanced Glaucoma Tests
Stereoscopic Optic disc photograph is taken as a baseline
It is a noninvasive imaging test used to evaluate the structural damage due to glaucoma. It rapidly takes cross sectional images of the optic nerve and retinal nerve fibre layer (RNFL) and helps in distinguishing between healthy and glaucomatous eyes. It is very useful for early diagnosis and follow up of glaucoma cases.
This is an automated test of the field of vision and helps to detect any loss or blind spots. It is the gold standard test for diagnosis and progression of glaucoma. It is performed in a dark room, the eye being tested focuses on a central target while dim lights appear at different areas of the bowl and one has to press a button to indicate when you see the light. The test has a learning curve and needs to be repeated at least once a year.
Stereoscopic Optic disc photograph is taken as a baseline
It is a noninvasive imaging test used to evaluate the structural damage due to glaucoma. It rapidly takes cross sectional images of the optic nerve and retinal nerve fibre layer (RNFL) and helps in distinguishing between healthy and glaucomatous eyes. It is very useful for early diagnosis and follow up of glaucoma cases.
This is an automated test of the field of vision and helps to detect any loss or blind spots. It is the gold standard test for diagnosis and progression of glaucoma. It is performed in a dark room, the eye being tested focuses on a central target while dim lights appear at different areas of the bowl and one has to press a button to indicate when you see the light. The test has a learning curve and needs to be repeated at least once a year.
Can Vision be restored with Glaucoma treatment?
Unfortunately, vision lost as a result of Glaucoma is usually permanent and cannot be restored. Most cases of Glaucoma, if diagnosed and treated early, enjoy a normal life. Once diagnosed as a glaucoma patient, you need regular monitoring. It can be successfully controlled with medicines, eyedrops, laser or surgery.
What are the Types of Glaucoma?
Angle Closure
The drainage pathways for the fluid (Aqueous humour) formed within the eye is narrowed leading to increased back pressure.It often presents as a sudden attack of Glaucoma with very high pressure, can cause severe headache, pain, nausea and loss of vision.
Open angle
The angle is not obstructed by iris tissue but there is resistance in the outflow channels. It starts gradually, is painless with no warning symptoms.
Normotensive/ Low tension
Despite normal eye pressure, there is damage to the optic nerve usually due to less blood supply and low blood pressure
Congenital
It presents early in life and is due to defective development of normal drainage structures in the eye. Babies born with it may have cloudy eyes, watering and light sensitivity.It usually needs early surgery.
Traumatic
Eye injuries can lead to glaucoma due to bleeding or scarring that obstructs the outflow of fluid
Neovascular
Serious and intractable form of glaucoma due to growth of abnormal blood vessels on the iris.
Secondary
Glaucoma can occur due to other eye diseases such as mature cataract, eye inflammation, eye tumours, eye surgery, medications etc.
How is Glaucoma treated?
In the early stages there are no obvious symptoms. By the time the patient becomes aware of decreased sight, the damage is already quite advanced. Hence, it is important to have regular eye check ups especially over the age of 40 years. Depending on the type of Glaucoma ( Open or Closed angle) following symptoms may occur


Medication Tips
- Make a medicine schedule
- Use only one drop at a time
- Apply pressure for 30 seconds over the tear duct near the inner corner of eye
- Keep a gap of at least 10 min between 2 eye drops
- In case you miss an eyedrop, use it at the earliest possible time
- Inform your doctor about any side effects
- Regular treatment and follow up is essential

